Raising Awareness around Maternal Mental Health, By Catia Marques and our D&I committee
This May, we are spreading the word about Maternal Mental Health Awareness Month. As with many mental health issues, maternal mental health (MMH) has historically gone under the radar, leaving sufferers with limited support. To help combat that, we have written this blog to shine a light on the issues, how to address them and direct those in need of support to the best resources we’ve found on the subject.
What is Maternal Mental Health?
The World Health Organization (WHO) describes MMH as “a state of well-being in which a mother realizes her abilities, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to her community”. However, other studies note that mental health is not the same as the absence of mental illness but reflects a capacity to adapt and cope.
MMH disorders include Depression, anxiety, OCD, PTSD, Bipolar and substance abuse. These disorders and symptoms often occur during pregnancy and, or during, the postpartum period (together often referred to as the perinatal period). Maternal mental health disorders not only affect mothers, but also the physical and mental health and well-being of their partner and closest family.
Consequences of untreated MMH disorders
Mothers with an untreated MMH disorder are more likely to neglect their own health, experience various forms of abuse, have impaired mother-child interactions and become less responsive to the baby’s cues. Meanwhile, the child could be born with a low birth size, have a pre-term birth, stay longer in the neonatal intensive care unit (NICU), and experience behavioural, cognitive, or emotional delays, which can negatively impact their childhood and long-term health.
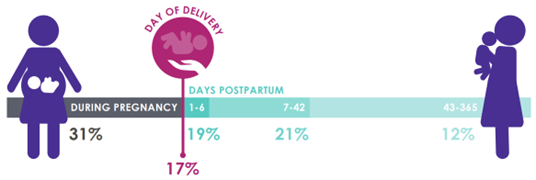
When all these factors come into play, the mother may begin to question their own competency and if the mental strain becomes too overwhelming, could potentially take their own lives. Most pregnancy-related deaths occur in the postpartum period (see below) and all these deaths are avoidable.
Treatments for MMH disorders
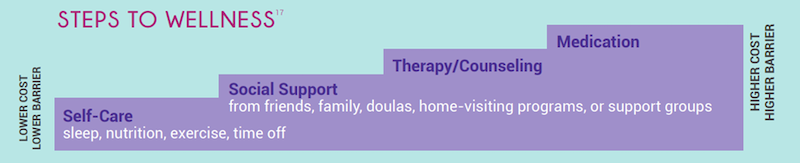
The good news is that most maternal mental health conditions are temporary and treatable. With that said, social isolation caused by the coronavirus pandemic can exacerbate feelings of loneliness. While new mothers in many countries and cultures are provided special care and consideration during the fourth trimester (180 – 365 days postpartum), the attention is usually directed towards the baby, not the mother. However, providers and policymakers alike are recognizing that new mothers need care and attention to recover from the physical and emotional aspects of pregnancy, childbirth, and new parenthood.
To benefit the health of women and infants, postpartum care should be an ongoing process, rather than a single encounter, with services and support tailored to each woman’s individual needs. Soon to become parents need to do postpartum planning: much like a birth plan helps expectant parents think through labour and delivery, a postpartum plan can help them think about the first few weeks with a new baby. Topics to ponder over include sleep, infant feeding, care for other children, meals, and more. Partner support during the postpartum time is essential for women’s recovery.
Peer support is a notable example of a social support group that has been verified as a vital way of addressing behavioural health. Peer support occurs when people provide knowledge, experience, emotional, social or practical help to each other. Nothing says “we are all in this together” quite like a community in similar situations sharing lived experiences!
Studies back up this claim too; according to Mental Health America, peer support programs increase social support and participation in the community, improve well-being, decreases length of hospital stays and encourages more thorough and longer-lasting recoveries.
What’s more, it can be a very lonely and isolating time for new mothers and peer support can provide opportunities to connect with others sharing similar emotions. Being aware that other new mothers are coping with anxiety and/or depression can be reassuring and validating. Best of all, peer support doesn’t is free to access, provides non-judgemental spaces, increases access to care and fills gaps in mental healthcare.
What Eigen is doing to support Mothers Mental Health
Here at Eigen, we understand work-life balance strategies are essential to reduce the distress associated with the return to work and to promote wellbeing in the perinatal stage. We have Employee Assistance Programs (EAPs) available in the US, UK and Portugal: TalkSpace (via Justworks) for employees in the US, Medicash for employees in the UK and ifeel for employees in Portugal.
For additional support, we provide a directory of links to third-party organizations based in the US, UK and Portugal that can provide MMH assistance, including helplines, peer-to-peer communication channels, and other maternal support services.
US-Based Resources:
- Postpartum Support International
- New Mom Health
- Dona International (Certified doulas; postpartum plan)
Here are some useful resources based in the UK:
- Maternal Mental Health Alliance
- Netmums (chat, guidelines & tips for trying for a baby, pregnancy, new parents, baby, etc.)
- (APP) Action on Postpartum Psychosis
Resources in Portuguese:
- Apoio à Vida (free helpline for pregnant and soon to become mothers)
- Mamãs e Bebés (Community + Blog)
- Rede Portuguesa de Doulas (doulas network)
As well as the formal support we provide to all our people, Eigen has fantastic communities that are a great place to go for advice and guidance. We have #mothers and #dads community channels within our Slack workspace and they are great places to go to for support, advice, cute photos, and bad jokes!
With increased awareness surrounding MMH, we can remove the stigma around the subject, provide access to the right mental health resources and let more mothers know there is an abundance of support available to guide them on their journey.

-
World Economic forum 2020
-
Gartner Cool Vendor 2020
-
AI 100 2021
-
Lazard T100
-
FT Intelligent Business 2019
-
FT Intelligent Business 2020
-
CogX Awards 2019
-
CogX Awards 2021
-
Ai BreakThrough Award 2022
-
CogX Awards Best AI Product in Insurance
-
FStech 2023 awards shortlisted
-
ISO27001
-
ISO22301
-
ISO27701
-
ISO27017
-
ISO27018


















